Running with heel pain can be an excruciating experience. If you have an active lifestyle, it’s difficult to adjust your routine to limit your physical activity once you encounter heel pain. This makes it important to know the symptoms and treatment methods for some of the most common types of heel pain that develop among runners. Understanding the types of running injuries is the key to effective treatment.
Plantar Fasciitis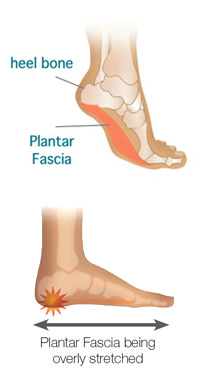
Plantar fasciitis is a painful inflammation of the plantar fascia – a thick, fibrous band of connective tissue in the sole of the foot that supports the arch of the foot. It runs from the ball of the foot to the heel, stretching to its limit when the foot is on the ground and supporting your full body weight. When placed under excessive stress, the plantar fascia stretches too far and tears, resulting in inflammation. The effects of the stress can build up gradually or be the result of a sudden incident.
Plantar Fasciitis is a common type of heel pain among runners for a number of reasons. Runners often have exercise routines that are simply too long, and too stressful on the feet and plantar fascia, especially for those individuals who suffer from flat feet. Combined with shoes that lack proper arch support, running routines that are too extensive put repetitive stress on the plantar fascia, particularly where it connects to the heel, causing tears in the fibers and resulting in inflammation and severe pain.
The most common causes of Plantar Fasciitis include:
- sudden increase in activity such as running or sports
- weight gain
- excessive pronation
- poorly fitting footwear and deficient arch support
Heel pain is commonly felt on the bottom of the foot, where the plantar fascia attaches to the heel bone. Typically the pain is most severe in the mornings when getting out of bed, because the fascia shortens and tightens while you sleep. When you stand up, the sudden stretch and load of your body weight pulls on the attachment to the heel bone. Symptoms of plantar fasciitis vary from mild to severe. They can linger for months at a time, with pain increasing and decreasing in an unpredictable pattern. Often, the pain disappears for several weeks,only to re-emerge full-blown after a single workout or change in activity.
The pain may even temporarily fade as you walk. Plantar Fasciitis is a common condition that runners experience, and along with the causes listed above, can be triggered by a sudden increase in your training schedule, or by switching running surfaces, especially when going from a softer surface to a harder one.
While Plantar Fasciitis can be treated, it does not heal quickly. It is recommended that you review each of the factors in order to avoid it. Most sports physiotherapists recommend the following approach to prevent Plantar Fasciitis:
- Stretch - before, during, and after activity. Tight calf and/or hamstring muscles (back of thigh) limit range of motion and put extra strain on the plantar fascia. Stretching as a warm up and as a cool down will help you move easily, keep muscles flexible and relaxed, joints mobile and relieve tension and strain. Performing plantar fasciitis exercises to stretch the plantar fascia is highly recommended.
- Footwear and orthotics – Ensure you have good footwear. More severe cases will benefit from wearing orthotics inside the shoes to improve foot biomechanics. Going barefoot is a bad idea, even at home. Avoid worn-out shoes and try running on soft surfaces.
- Change your level of activity – You don’t have to stop exercising, however consider switching to a non-weight bearing sport like swimming or cycling. When you do try running again, begin at a much lower level of intensity and a shorter distance, then you can build up gradually. reduce the volume or intensity of training, or simply reduce the amount of time spent on your feet.
- Ice – Icing the heel area will help decrease the inflammation and pain. Put your foot on a frozen bottle of water or a bag of frozen peas wrapped in a towel, 3 or 4 times a day for 5-10 minutes each time. Never ice more than once an hour to prevent risk of ice burn to desensitized tissue.
If the problem persists, talk to a podiatrist or physiotherapist.



 100% Secure
100% Secure

{ 0 comments… add one }